In the medical device industry, where patient safety is paramount and commercialization pressures are relentless, development teams must perform a masterful tightrope walk. They must balance two seemingly conflicting design principles: Design for Manufacturability (DfM) optimizing for cost-effective production and Design for Reliability (DfR) ensuring durable and safe performance throughout the product's lifecycle.
This is not merely a trade-off; it is a complex, multivariate optimization problem. A single misstep can create a ripple effect, impacting the bill of materials (BOM) cost, time-to-market, regulatory compliance, and ultimately, brand reputation.
This article will perform a deep analysis of the anatomy of these trade-offs through specific technical scenarios and propose a strategic framework for product managers and engineers to navigate this challenge confidently, turning potential conflict into a symbiotic partnership.
Redefining the Playing Field: Moving Beyond Unit Cost to Total Cost of Ownership (TCO)
The classic confrontation between DfM and DfR stems from a difference in reference frames:
- DfM focuses on CAPEX and Production Costs: The goal is to minimize BOM costs, shorten assembly cycle times, and optimize for high-volume automated manufacturing processes. Success is measured by metrics like yield rate, cost per unit, and throughput.
- DfR focuses on OPEX and Risk Management: The goal is to minimize field failure rates, warranty costs, the risk of product recalls, and potential legal liabilities. Success is measured by metrics like Mean Time Between Failures (MTBF), operational lifetime, and, most importantly, the absence of adverse events related to patient safety.
A decision that focuses solely on trimming 5% from the BOM cost could lead to a 200% increase in warranty and post-market support expenses. Therefore, shifting the mindset from manufacturing cost to Total Cost of Ownership (TCO) is the first and most critical step. TCO encompasses all costs from R&D, production, deployment, and maintenance to end-of-life.

Anatomy of the Trade-offs: A Deep Technical Analysis
Let's dissect real-world situations to clearly see the tension between DfM and DfR.
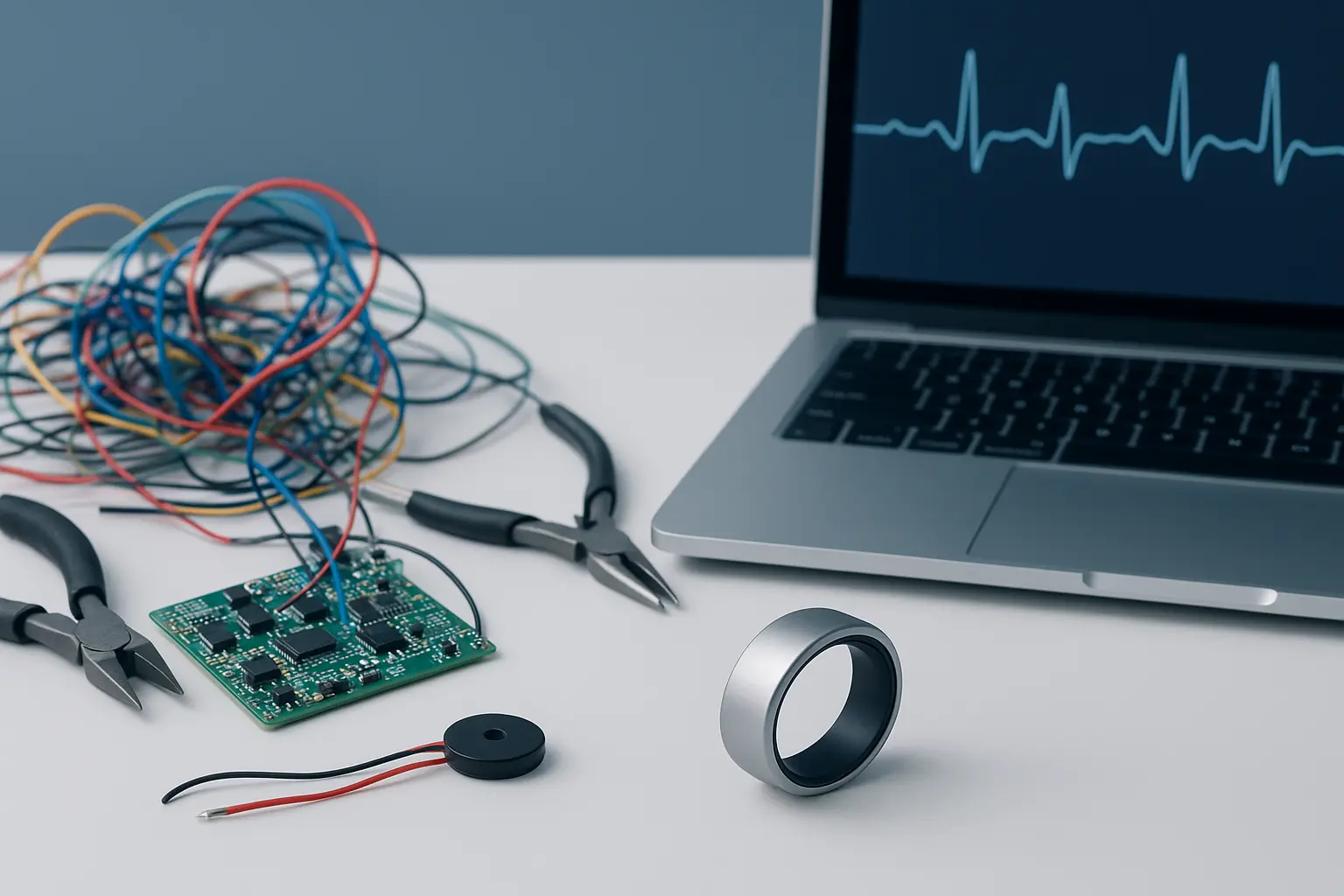
Scenario 1: Enclosure Materials for a Wearable Vital Monitor
- Situation: A wearable device for monitoring ECG and SpO2 requires an enclosure that is durable, lightweight, and biocompatible per ISO 10993 standards.
- The DfM Perspective: Select a standard medical-grade ABS or Polycarbonate (PC) plastic. These materials are low-cost, widely available, and easy to process in high-speed injection molding.
- The Hidden DfR Risk: In a hospital environment, this device will endure repeated cleaning cycles with harsh chemical disinfectants like 70% isopropyl alcohol or quaternary ammonium compounds. These standard plastics, while biocompatible, are highly susceptible to Environmental Stress Cracking (ESC). Over time, microcracks will form, compromising the enclosure's Ingress Protection (IP) rating, allowing moisture to seep in and damage the internal electronics. Furthermore, these materials may not be compatible with advanced sterilization methods like Gamma or EtO if the device needs to be supplied sterile.
- The Strategic Balance: Conduct material selection analysis based on real-world use cases. An engineered polymer like PSU (Polysulfone) or PEI (Polyetherimide) might have a 20-30% higher material cost but possesses superior chemical and heat resistance, ensuring the device's integrity over its projected 5-year lifecycle. The added investment in materials is offset by a significant reduction in warranty claims and recall risks.
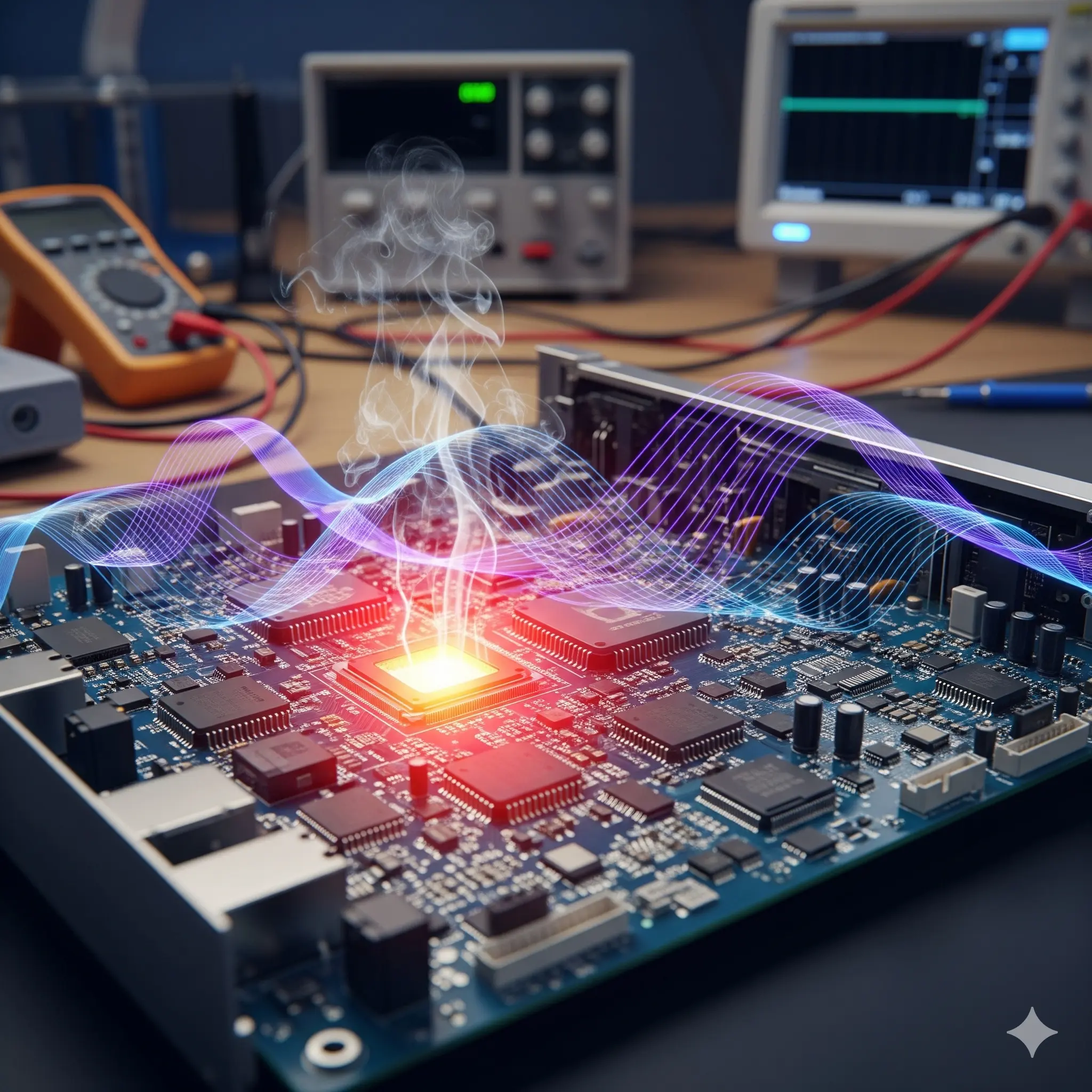
Scenario 2: PCB Design for a Mixed-Signal Diagnostic Device
- Situation: A handheld diagnostic device uses a sensitive biosensor (the analog part) and a powerful microprocessor for on-device data analysis (the digital part).
- The DfM Perspective: To reduce size and cost, engineers lay out components on a dense, 4-layer Printed Circuit Board (PCB). This reduces the cost of the PCB material and allows for a more compact and cheaper enclosure.
- The Hidden DfR Risk: This design creates two severe problems:
- Crosstalk: High-speed digital signal traces from the processor can induce Electromagnetic Interference (EMI) in the highly sensitive Analog Front-End (AFE) circuits, which are processing biological signals at the microvolt level. This results in corrupted measurements and, consequently, incorrect diagnoses.
- Inefficient Thermal Management: Placing the processor and power modules too close together without an adequate thermal ground plane creates hotspots. This not only shortens the lifespan of those components (thermal derating) but can also affect the accuracy of nearby temperature-sensitive sensors.
- The Strategic Balance: Strictly apply mixed-signal PCB design rules. This might involve using a 6-layer PCB to incorporate dedicated ground and power planes, creating physical isolation between analog and digital zones, and using shielding techniques. Concurrently, perform thermal simulations early to optimize component placement and heatsink design. The PCB cost may increase by 15%, but the accuracy and reliability of the measurement the core value of the product are preserved.
Scenario 3: Software Library Selection for Device Firmware
- Situation: The firmware for an infusion pump requires a complex algorithm to control a stepper motor.
- The DfM Perspective (for software development): Use a popular, community-vetted open-source library for motor control. This significantly shortens development time and R&D costs.
- The Hidden DfR Risk: This is a Class II medical device, and its firmware must adhere strictly to the IEC 62304 standard. An open-source library, while functional, typically does not come with the complete set of test documentation, risk analysis, and version history required by IEC 62304. The effort to "qualify" this library (recreating documentation, performing unit tests, code reviews) for an FDA submission could be more costly and time-consuming than developing it in-house. Moreover, latent, undiscovered bugs in the library could lead to critical safety failures.
- The Strategic Balance: Assess the risk of SOUP (Software of Unknown Provenance) from the outset. If the library serves a non-critical function, its use may be acceptable with appropriate controls. However, for a safety-critical function like infusion pump control, the safer choice is to invest in a commercial RTOS (Real-Time Operating System) that is already IEC 62304 certified, or to allocate the resources to develop and validate an in-house library according to the proper process.
A Strategic Framework for Optimal Balance: The Holistic DfX Approach
To navigate successfully, organizations need a structured methodology. This isn't just about DfM or DfR; it's about Design for Excellence (DfX), an integrated philosophy.
- Phase 1: Integrated Risk & Requirements Modeling:
- Establish a cross-functional team (design, manufacturing, quality, supply chain, regulatory) from day one.
- Use Failure Mode and Effects Analysis (FMEA) not only to identify risks in the design (dFMEA) but also in the manufacturing process (pFMEA). Directly link product requirements to potential failure modes.
- Phase 2: Quantitative Decision Analysis:
- Build a weighted decision matrix for critical design choices.
- Evaluation criteria should include: BOM cost, assembly time, impact on yield rate, projected MTBF, supply chain complexity (e.g., single-source components), and regulatory compliance risk. Assign weights to each criterion based on the product's business strategy.
- Phase 3: Accelerated Testing & V&V Loops:
- Don't wait for the final validation stage. Perform Highly Accelerated Life Testing (HALT) on early prototypes to proactively find design weaknesses.
- Data from HALT provides invaluable information to strengthen the design, e.g., "Component C failed after 20 hours at 85°C; we need to source an alternative with a wider operating temperature range."
- Phase 4: Design for Supply Chain (DFSC) Integration:
- A manufacturable and reliable design is meaningless if key components have a 52-week lead time or come from a single supplier in a geopolitically unstable region.
- Work with the supply chain team early to ensure that selected components not only meet technical specifications but are also readily and reliably available from multiple sources.
Conclusion: DfM and DfR. A Symbiotic Partnership
Viewing DfM and DfR as opposing forces is a strategic error. In modern medical device development, they must be a symbiotic partnership. The most reliable design must be manufacturable to reach the market. The most manufacturable design must be reliable to earn and maintain trust.
Success lies in building an engineering culture where every design decision is viewed through both lenses. By implementing a systematic DfX framework, leaders can guide their teams to create products that are not only technologically innovative but also technically robust, safe for patients, and commercially